Todd Baron, MD is a Gastroenterologist and Professor of Medicine at the University of North Carolina, School of Medicine. He also serves as the Director of Advanced Therapeutic Endoscopy within UNC's Division of Gastroenterology and Hepatology.
In this blog, Dr. Baron presents a case of a 66-year-old patient who underwent a Whipple operation to treat adenocarcinoma of the pancreatic head. Post-surgery, she presented with a malignant biliary obstruction, requiring a second endoscopic retrograde cholangiopancreatography (ERCP) due to the obstruction hindering the first procedure’s success.
Using the following approach, Dr. Baron was able to achieve precise stent placement below the bifurcation and provide relief for his patient.
ENDOSCOPIC INTERVENTION
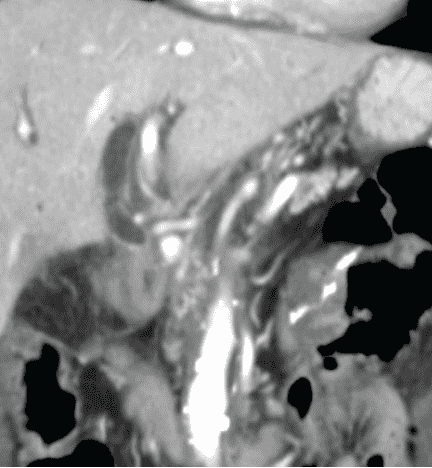
The endoscope was passed into the afferent limb, but the biliary anastomosis (hepaticojejunostomy) was obstructed. An Endoscopic Ultrasound-guided Rendezvous (EUS-RV) technique was performed using a therapeutic channel linear echoendoscope initially to view the obstruction. The left hepatic duct was punctured with a standard 19 gauge EUS Aspiration Needle and a cholangiogram showed obstruction of the common hepatic duct (Figure 2).
Figure 2: Coronal computed tomography (CT) prior to endoscopic intervention showing dilated biliary tree with obstruction at the hepaticojejunostomy by soft tissue mass
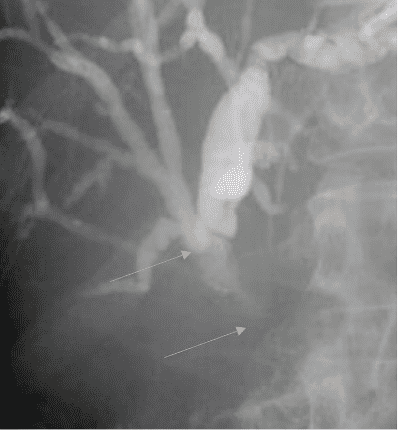
A 450cm long guidewire was passed antegrade into the biliary tree, across the hepaticojejunostomy and into the jejunum (Figure 3).
Figure 3: Radiographic image showing echoendoscope in the stomach with injection via 19 gauge endoscopic ultrasound aspiration needle after puncture of the left hepatic duct. Cholangiogram shows dilated intrahepatic duct with obstruction at the hepaticojejunostomy. The top arrow points to the bifurcation. Bottom arrow points at the upper margin of stricture.
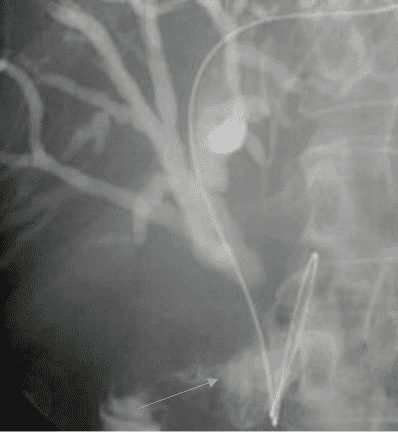
The forward viewing endoscope was reintroduced, and the guidewire was grasped and withdrawn through the endoscope (Figure 4).
Figure 4: Radiographic image showing the guidewire passed through the needle across the hepaticojejunostomy into the jejunum. The arrow points to the contrast in jejunum.
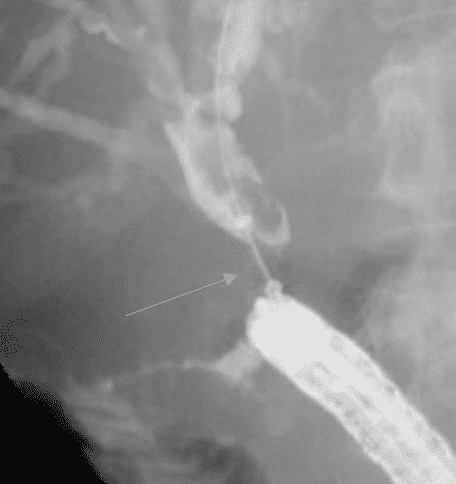
Over the guidewire, a 10mm diameter X 4cm length GORE® VIABIL® Biliary Endoprosthesis was placed via ERCP with the proximal end just below the biliary bifurcation (Figures 5 and 6).
Figure 5: Radiographic image showing forward-viewing endoscope positioned in the jejunum with guidewire grasped. The arrow points at midpoint of stricture.
Figure 6: Radiographic image showing GORE® VIABIL® Biliary Endoprosthesis in place immediately after deployment. A waist is seen in the center of the stent at the point of stricture. The arrow points to the stent waist.
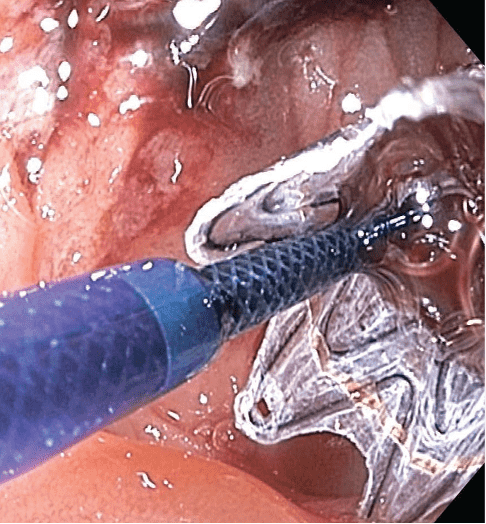
The distal end of the GORE® VIABIL® Biliary Endoprosthesis was placed in the duodenum (Figure 7).
Figure 7: Endoscopic image of GORE® VIABIL® Biliary Endoprosthesis immediately upon deployment with endoscope positioned in the jejunum, just distal to the hepaticojejunostomy.
POST-TREATMENT OUTCOME
The second ERCP and placement of the GORE® VIABIL® Biliary Endoprosthesis resulted in successful relief of the biliary obstruction with normalization of serum bilirubin. Two months post-procedure, the serum bilirubin remained normal.*
“I trust in the GORE® VIABIL® Biliary Endoprosthesis.” Dr. Baron shared. “The features it possesses that are important to me include: the anti-migration properties, which are proven, the lack of foreshortening during and after deployment, the ability to precisely place because the stent is directly deployed from the catheter rather than being expelled out of a sheath, and it’s conformability to the biolung.”
* This patient later died due to complications from the progressive malignant disease.