Bone Void Fillers
Versatile Solutions for Bone Graft Defects

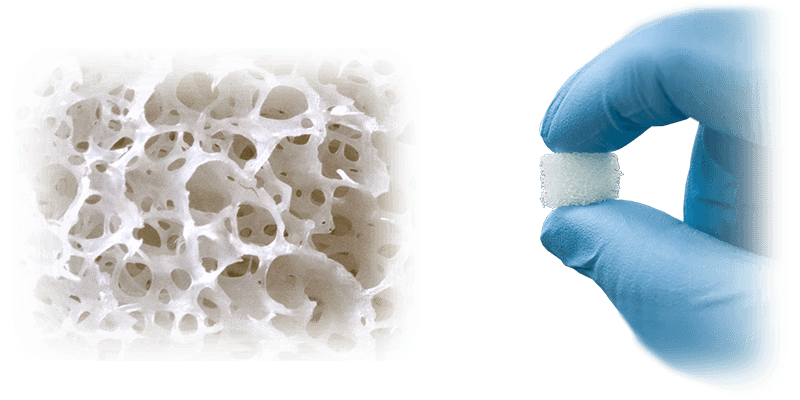
AlloAid® BP
This demineralized bone matrix (DBM) putty is a moldable and flowable allograft intended for the filling of bony voids or gaps that are not intrinsic to the stability of the bony structure. It is both osteoconductive and osteoinductive, supporting new bone formation during the natural healing process. The putty is suitable for use in bone regeneration procedures and may be combined with autologous bone marrow aspirate or platelet-rich plasma to create a composite graft with enhanced biological activity.
AlloAid® BP is available in flowable, formable putty, and crunch formats (DBM putty + cortical cancellous bone chips). Made from 100% human bone, it is sterile—gamma irradiated to SAL 10⁻⁶— and stores at ambient room temperature. Donor recovery and screening are performed according to FDA and AATB guidelines.
BioV® Bioactive Matrix
This composite graft material combines bioactive glass and demineralized bone matrix (DBM) to fill non-structural bony voids or gaps that are not intrinsic to the stability of the bony structure. The formulation provides both osteoconductive and osteoinductive properties supporting new bone formation during the natural healing process.
The material is moldable and extrudable, resists migration under irrigation, and may be used in conjunction with autograft as a bone graft extender. Sterilized by e-beam irradiation to a SAL of 10⁻⁶, the product is available in 1cc, 2cc, 5cc, and 10cc formats.
BIOV® BP complies with all FDA, AATB, and State Regulatory requirements for donor screening, recovery, and testing.
Tribio® Backfill Plugs
This sterile, ready-to-use bone void filler is intended for the filling of bony voids or gaps that are not intrinsic to the stability of the bony structure. It may be used in surgically created or trauma-induced osseous defects and can be combined with autograft or bone marrow aspirate to enhance biological activity.
The formulation consists of hydroxyapatite (HA), tricalcium phosphate (TCP), and bioactive glass within a collagen matrix, providing an osteoconductive scaffold that rapidly absorbs blood and fluids to support new bone formation. The material is biocompatible and resorbs over time as it remodels into native bone, forming a calcium phosphate layer similar to natural bone mineral. The product is available in preformed plug sizes (5.5 mm × 40 mm and 7.5 mm × 40 mm) for ease of placement and optimal fit.
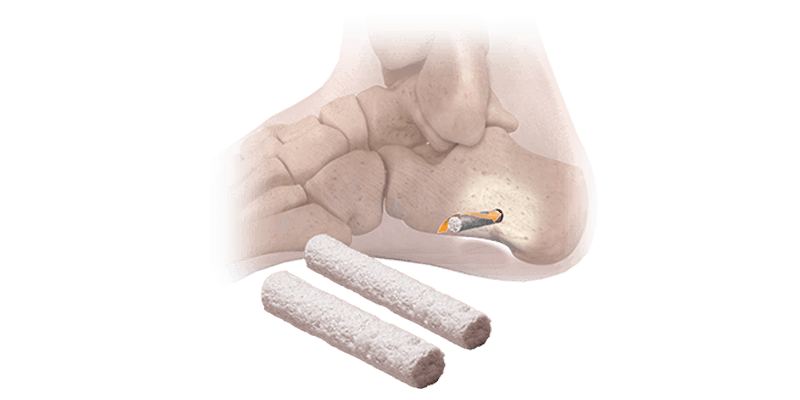
AlloAid® Backfill Plugs
This resorbable allograft is composed of 100% human cortical bone and is intended for the filling of bony voids or gaps that are not intrinsic to the stability of the bony structure, including those resulting from surgically created procedures or trauma. The graft is trimmable and tapered to facilitate insertion and may be gently packed into the defect site.
During the healing process, the graft resorbs and is gradually replaced by new bone. At the discretion of the clinician, it may be combined with autologous bone marrow to enhance biological activity. The graft is provided saline-packed and terminally sterile, with each pack containing a single implant measuring 2.2 mm × 30 mm.
AlloAid® Backfill Plugs complies with all FDA, AATB, and State Regulatory requirements for donor screening, recovery, and testing.
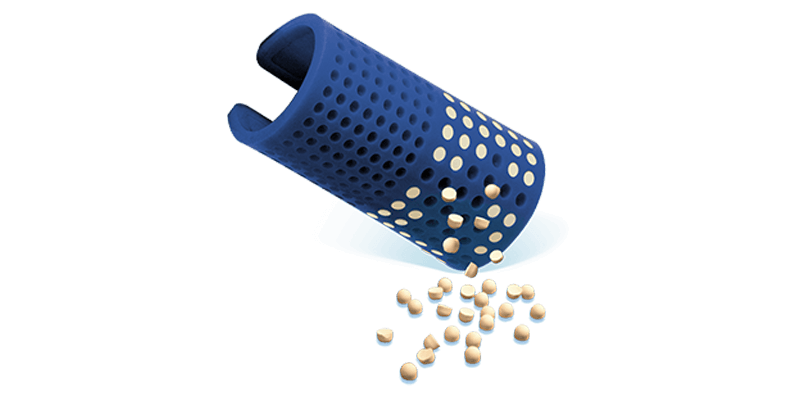
i2b™ Resorbable Bead Kit
This synthetic, resorbable bone void filler is intended for the temporary support and filling of non-structural bony voids or gaps that are not intrinsic to the stability of the bony structure. The formulation consists of a tri-blend of calcium sulfate, tricalcium phosphate, and hydroxyapatite, providing osteoconductive and biocompatible properties to support bone regeneration. The material is 100% synthetic, eliminating the risk of disease transmission, and is fully resorbable, gradually being replaced by natural bone during the healing process.
The product is moldable, radio-opaque, and may be formed into beads to fit the shape of the defect for direct placement. The material begins to harden within 2 minutes and fully sets within 5 minutes. The i2b™ Resorbable Bead Kit is sterile and contains bone void filler powder, sterile water, a spatula, and a bead mat. Available in 5g and 10g kit sizes.

Revision Core
This dense cancellous bone core is available in multiple diameters with cannulation to allow exact placement within the femoral and tibial tunnels. It’s also used to fill bone voids in small joint procedures.

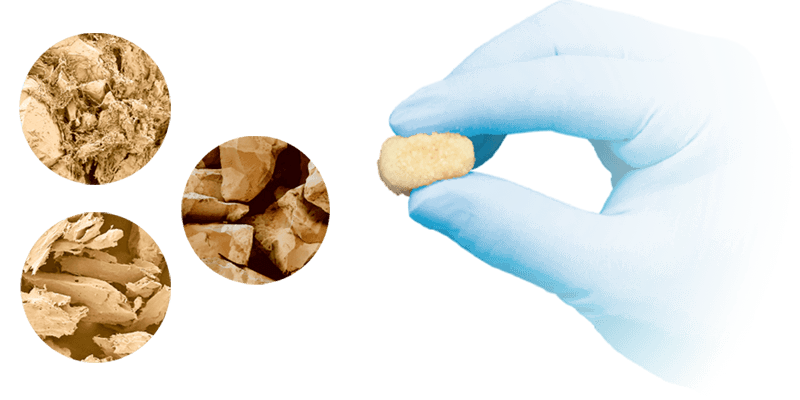
ENHANCE® Demineralized Cortical Fibers
This versatile filler is comprised of 100% demineralized cortical bone milled into a fibrous structure. It handles like a DBM putty and offers the ability to customize the rehydration process with BMA, PRP, whole blood, or saline. In pre-clinical models, ENHANCE® has been shown to provide consistent osteoinductive potential at higher levels than observed in alternate bone graft options.1
1 Data on File, MTF Biologics
Experience the Difference

