Imagine this scenario…
A young female collegiate soccer player arrives at the surgery center first thing in the morning for a primary ACL Reconstruction. On top of suffering through the pain of the initial injury, she’s also dealing with the isolation of being away from her team and worrying about her scholarship. Now, she is mentally and physically preparing herself for surgery and the long rehabilitation process that is required, all in hopes of returning to the field and playing the sport she loves.
She and her parents are having pre-operative discussion with her surgeon, listening and agreeing to a list of potential medical devices that could be used during her procedure. She is hearing all that may occur during the operation, including the possibility of the surgeon using a cadaver graft instead of her own tendons to recreate her ACL.
|
The next thing she knows, she’s being wheeled into the procedural room with strange equipment and people hustling around preparing the room. Thankfully, her anxiety is “put to bed” as the anesthesia takes effect. |
 |
The OR clock has officially started...
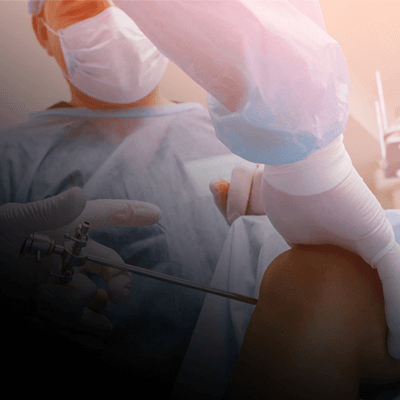
The surgeon starts the procedure and is disappointed to discover the patients hamstring tendons are quite small, measuring about 6mm, which according to literature reports less than optimal outcomes.1
Next, the surgeon pauses the procedure and makes a request for an allograft. Once received, the allograft is unwrapped and placed in Vancomycin for a few minutes to thaw, and the graft preparation on the patient may now start.
While all this has been occurring, the surgery has stopped. With this case taking longer than anticipated, adjustments will need to be made to all other cases scheduled for that room. In turn, breaks for employees will be altered and the possibility of working overtime is looming.
|
The case finishes smoothly, but the surgeon knows the use of an allograft in a young female is not the best scenario for graft incorporation.2 Now, the surgeon is going to have to monitor this patient more closely through physical therapy. Although a good surgical outcome, the long-term healing and strength of the reconstruction is questionable – not a good feeling for the surgeon considering this is a high-level student athlete. |
 |
What if there was another alternative?
Something that would be faster for the OR and allow the patient to utilize their own tissue?
Imagine this same scenario with one small difference…
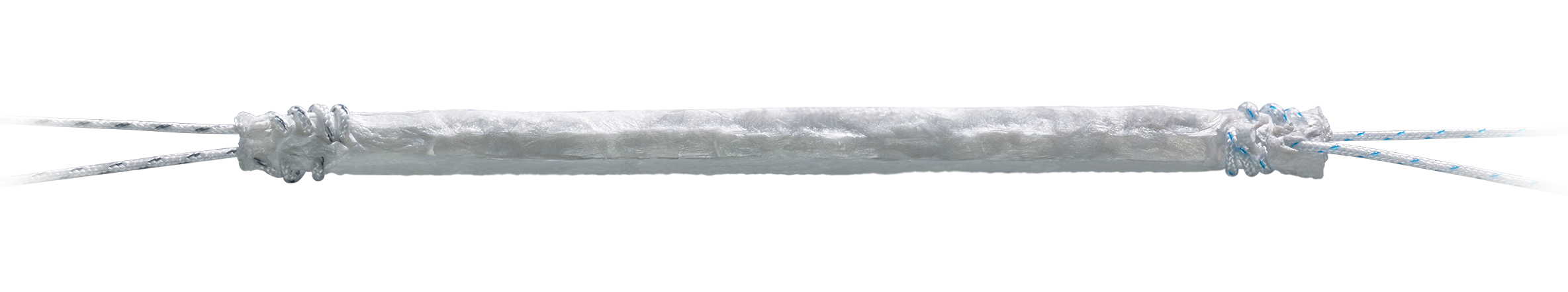
Once the surgeon realizes the autograft is small, she asks for the BioBrace® 5x250 Reinforced Implant - an off-the-shelf, no defrosting time needed implant designed to optimize soft tissue healing through augmentation.
In a matter of minutes, the package is opened and BioBrace® is incorporated into the standard graft preparation process without the addition of extra time. The surgeon is pleased with the size of the augmented graft, containing added collagen that is anticipated to aid in the incorporation of the autograft to bone - all while providing additional strength to the graft construct.
This leads to minimal OR delay, a low chance of employees working overtime, the surgeon is happy with the result and the patient is comfortable knowing she has her own tissue in her knee.
Learn more about augmenting soft tissue repairs with BioBrace®
1 Conte, Evan J., et al. "Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure." Arthroscopy: The Journal of Arthroscopic & Related Surgery 30.7 (2014): 882-890.
2 Kaeding CC, Pedroza AD, Reinke EK, Huston LJ; MOON Consortium; Spindler KP. Risk Factors and Predictors of Subsequent ACL Injury in Either Knee After ACL Reconstruction: Prospective Analysis of 2488 Primary ACL Reconstructions From the MOON Cohort. Am J Sports Med. 2015 Jul;43(7):1583-90. doi: 10.1177/0363546515578836. Epub 2015 Apr 21. PMID: 25899429; PMCID: PMC4601557.