We’re halfway through football season and knee injuries have been a persistent issue in the NFL - significantly impacting player performance and team dynamics. Last season, the league reported 52 ACL tears, a 24% decrease from the previous two seasons. But while ACL tears are decreasing, we're still seeing sidelined players with MPFL and other knee-related injuries. The high incidence of knee injuries remains a major concern for teams, players, and fans alike, highlighting the need for ongoing advancements in injury prevention and player safety protocols. A deeper understanding of the knee is essential for both proactive injury prevention and effective treatment after injuries occur.
The Complexity of the Knee
As we uncover the knee, we begin to realize just how intricate of a system it really is. The medial patellofemoral ligament (MPFL) is just one of the many roads in a highway system of soft tissue providing the knee with support and stabilization. The MPFL attaches anteriorly to the patella and posteriorly to the distal end of the femur. When we hear of knee injuries in sports medicine, the first things that comes to mind are the ACL or PCL, leaving you to wonder: How does someone ends up needing an MPFL procedure?
Leading Causes of MPFL Injuries
- Naturally loose ligaments (more common in females)
- Weakness in the muscles that support the knee
- Deformity of the femoral trochlea referred to as trochlear dysplasia
- Bony malalignments
- Previous knee dislocations
- Connective tissue disorder
MPFL Treatments
Once the conservative treatments like rest, ice, compression, and elevation (R.I.C.E.), as well as physical therapy, fail to resolve the issue, surgical approaches are then considered. There are four main procedures when it comes to surgical intervention:
- MPFL Repair – This method, as stated in the name, involves fixing the ligament. However, surgeons will typically recommend a reconstruction, as repair is usually saved for first-time acute injuries.
- MPFL Reconstruction – This method can utilize either an allograft or autograft and involves creating a new ligament all together
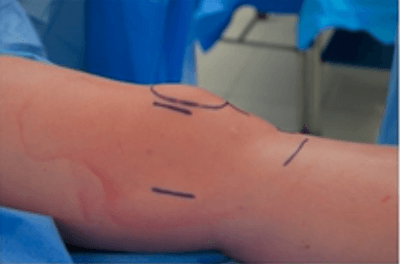
- Lateral Release & Medial Imbrication – Imbrication (to overlap) involves creating one or two incisions near the patella to tighten or loosen the ligaments depending on the anatomical needs of the patient to create normal patellar movement.
- Bone Realignment – Decreases the likelihood of dislocations and may be recommended when the patient has an abnormal anatomy of the knee where the tibial tubercle needs to be repositioned.
Solutions for MPFL Reconstruction
CONMED’s PopLok® is an ideal choice when opting for MPFL Reconstruction. The all-PEEK Knotless Suture Anchors provide reliable and reproducible tendon-to-bone fixation, attaching to the central part of the anchor. The anchor's innovative design allows surgeons to adjust suture tension once the anchor is seated in the pilot hole, offering maximum flexibility. A unique suture locking mechanism traps suture within the anchor, resulting in dependable fixation that is less dependent upon bone quality. The 3.5/4.5mm anchor design features wings that are deployed subcortically to provide secure fixation in the bone. A 2.8/3.3mm anchor offering provides strength and reliability for instability repairs.
The MPFL graft requires firm fixation in the femoral tunnel. CONMED’s GENESYS™ Matryx® Interference Screw delivers strong initial fixation during the critical healing period and provides a scaffold to enable bone in-growth during the subsequent resorption period. This process allows restoration of the patient’s natural anatomy both biologically and mechanically. These screws are comprised of CONMED’s proprietary GENESYS™ biocomposite material (a blend of microTCP and 96L/4D PLA), which clinical data has shown provides optimized absorption characteristics and proven bone in-growth.1
MPFL Function and Innovative Augmentation
The MPFL is critical in maintaining alignment of the patella, which mitigates patellar dislocations whether complete or partial (subluxation). Without an MPFL, the knee is prone to pain, mobility issues, and swelling. This ligament works to ensure the patella glides smoothly along the femoral grove during movement contributing to proper mechanical function within the knee. We can collectively agree that having full mobility and proper knee function is imperative to any athlete. Adapting to future needs in sports medicine, CONMED acquired a versatile solution with the ability to reinforce soft tissue (like the MPFL), allowing injured athletes to rebound with a stronger ligament and a quicker return to sports.
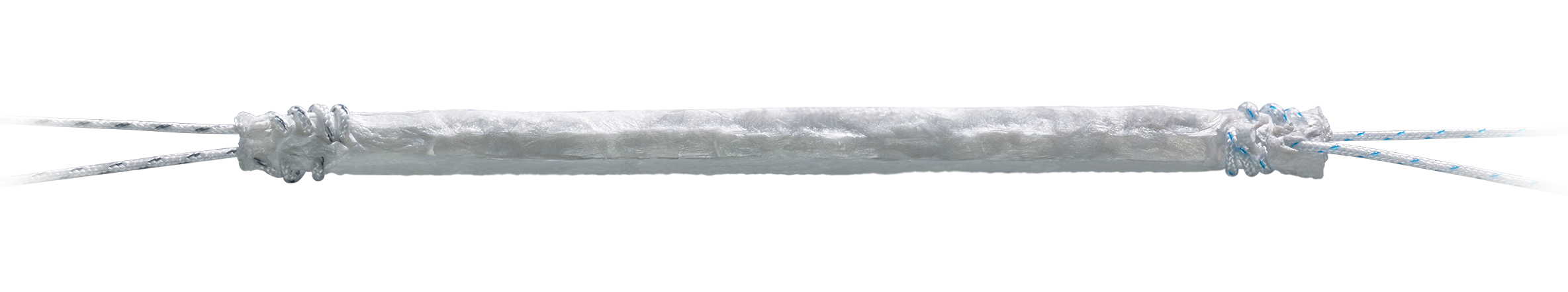
CONMED's BioBrace® Reinforced Implant is among the latest innovations in sports medicine, leading the charge in the augment space. BioBrace® is an FDA cleared implant indicated to reinforce soft tissue wherever weakness exists. It’s a highly porous, load-sharing, type 1 collagen sponge with PLLA microfilaments that provide the repair with structural report. The mechanical design allows for rapid cellular infiltration and host integration. BioBrace® provides supplemental strength for up to 2 years before naturally resorbing, making it a great option for a procedure like an MPFL repair or reconstruction. It’s the only augment that combines healing (type 1 collagen) and strength (PLLA microfilaments).2
Watch Dr. Hiemstra's MFPL Reconstruction Presentation
Enjoy this 4-minute excerpt on patellofemoral instability approaches.
Footnotes
1 Daculsi et al. Biomaterials 2011.
2 K203267 – 510(k) Clearance Letter - The BioBrace® Implant. Based on preclinical animal data
References
https://www.hss.edu/conditions_medial-patellofemoral-ligament-reconstruction-mpfl.asp
https://mskdoctors.com/doctors/charlotte-barker/articles/understanding-the-medial-patellofemoral-ligament-mpfl-and-its-crucial-role-in-knee-stability
https://alexanderorthopaedics.com/medial-patellofemoral-ligament-mpfl-reconstruction/#%3A%7E%3Atext%3DPrimary%20risk%20factors%20for%20experiencing%20a%20torn%20or%2Cvalgus%20alignment%2C%20femoral%20anteversion%2C%20or%20tibial%20external%20rotation