Last year, the guidelines for patient eligibility for bariatric and metabolic surgery were adjusted by the American Society for Metabolic and Bariatric Surgery (ASMBS) and the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO).
Motivated by hundreds of clinical studies and randomized trials, the move marks the first update to these guidelines in over 31 years. Read more on the adjusted guidelines here.
The prevalence of obesity is growing significantly. With 9.2% of Americans meeting morbid obesity criteria1 and two out of three U.S. adults classified as overweight or obese, many are looking to surgery as a solution for their weight loss goals and improved quality of life.
Surgical treatment has proven health benefits for those who meet the bariatric surgery requirements. And advances in minimally invasive techniques, like laparoscopic sleeve gastrectomy, have increased surgical demand…
But these procedures can present unique obstacles. Surgeons and anesthesiologists are looking for ways to overcome these challenges to continue to offer the care high BMI patients deserve.
Could a low pressure insufflation approach be part of the solution?
A growing number of publications have suggested that operating at low pressure during laparoscopic and robotic surgery can positively impact procedures.2,4,6
In this article, we’ll consider three common challenges that present in bariatric procedures and review the impact of a low pressure approach for each.
1. Many patients undergoing bariatric surgery tend to have comorbidities that can create mechanical ventilation challenges.2
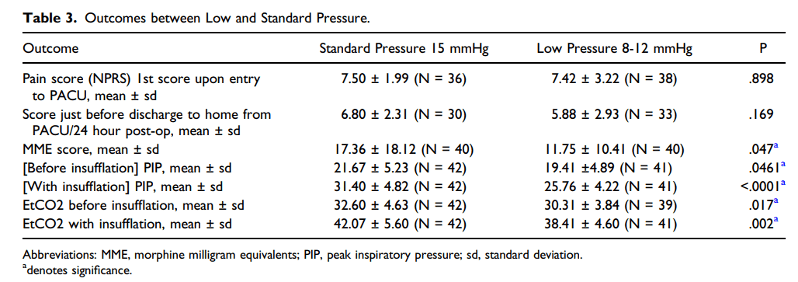
A recently published study observed the outcomes of low intra-abdominal pressure vs standard pressure to evaluate respiratory and other clinical impacts. The outcomes demonstrated significant reductions in both peak airway pressure and ETCO2 in the low pressure patient group.3
FINDINGS:3
- Mean peak inspiratory pressures during insufflation were significantly higher for procedures conducted at standard pressure (31.40 ± 4.82) compared to the 8 mmHg (24.68 ± 4.19) and 12 mmHg (27.33± 3.85) low pressure groups (one-way ANOVA, P < .0001).
- During insufflation, there was a significant increase in the average ETCO2 in the standard pressure group (42.07 ± 5.60) compared to the 8 mmHg low pressure group (37.59 ± 5.05) (ANOVA, P = .0096).
Also worth noting, the authors documented that “this study demonstrates that complex laparoscopic surgery can be accomplished under low pressure pneumoperitoneum (8-12 mmHg) with no detriment to the working field, intraoperative vision, smoke evacuation, and without increase in operative time.”
Dr. Gabriel Eduardo Mena, Professor for Department of Anesthesiology and Perioperative Medicine, University of Texas MD Anderson Cancer Center, shared his experience operating at low pressure with AirSeal®:
“I have noticed a significant decrease in peak inspiratory airway pressure and mean airway pressure while using the AirSeal system. These benefits are extremely important when taking care of obese patients who have increased airway resistance and decreased pulmonary compliance from baseline.”
2. Patients with increased adipose tissue can create exposure and visualization complications.
While laparoscopy is preferred over open surgery for high BMI patients, it can also prove more challenging due to higher amounts of intraabdominal fat which can add difficulty accessing and maintaining pneumoperitoneum.4 A study published in 2022, examined the impact of low-pressure insufflation, which included a group of women with a BMI > 30 mg/m2. Using 8-10 mmHg in a low pressure group, and 12-14 mmHg in a standard insufflation group, the authors aimed to document anesthesia parameters and post operative pain.
FINDINGS:5
- Patients in the AirSeal group recovered significantly faster compared to the standard group: 98% of women in the low pressure group were discharged within 2 days, compared to 75% of patients in the standard group (p < 0.0001). The subgroup of high BMI patients maintained these findings.
- The use of low-pressure insufflation with the AirSeal® system allowed for a significant limitation of the increase in ETCO2, peak airway pressure and maximum systolic blood pressure during surgery.
- The overall consumption of CO2 was also reduced with AirSeal® (35 L, IQR range 30–26) compared with traditional insufflation (50 L, IQR 40–50; p = 0.0001).
The authors also noted: “Adoption of a valveless [AirSeal] system also has the advantage of maintaining optimal exposure of the operative field even with a lower pressure of insufflation and allowing the continuous emission of surgical smoke.” 4
The rate of readmissions tends to increase in high BMI patients.
Studies show that readmissions can increase in overweight patients or patients with class I obesity, diabetes, and obstructive sleep apnea.3 In 2019, Drs. Ronney Abaza and Matthew Ferroni published a comparison of outcomes in patients who underwent robot-assisted laparoscopic prostatectomies.
Evaluating 300 RALP patients, whose body mass index ranged from 19.5–44.3 kg/m2, the authors documented pain scores, length of stay, and complications in groups who underwent surgery at 6 mmHg vs the standard 15 mmHg.